Platelet-Rich Plasma (PRP) and Bone Marrow Aspirate Concentrate (BMAC) are advanced, minimally invasive regenerative treatments that harness your body’s own healing potential. At our practice, we use ultrasound-guided injection techniques to deliver concentrated growth factors (PRP) or stem/progenitor cells (BMAC) directly to damaged tendons, ligaments or soft tissue around the elbow — helping reduce pain, stimulate tissue repair, and potentially avoid or delay surgery.
Cubital Tunnel Syndrome Report
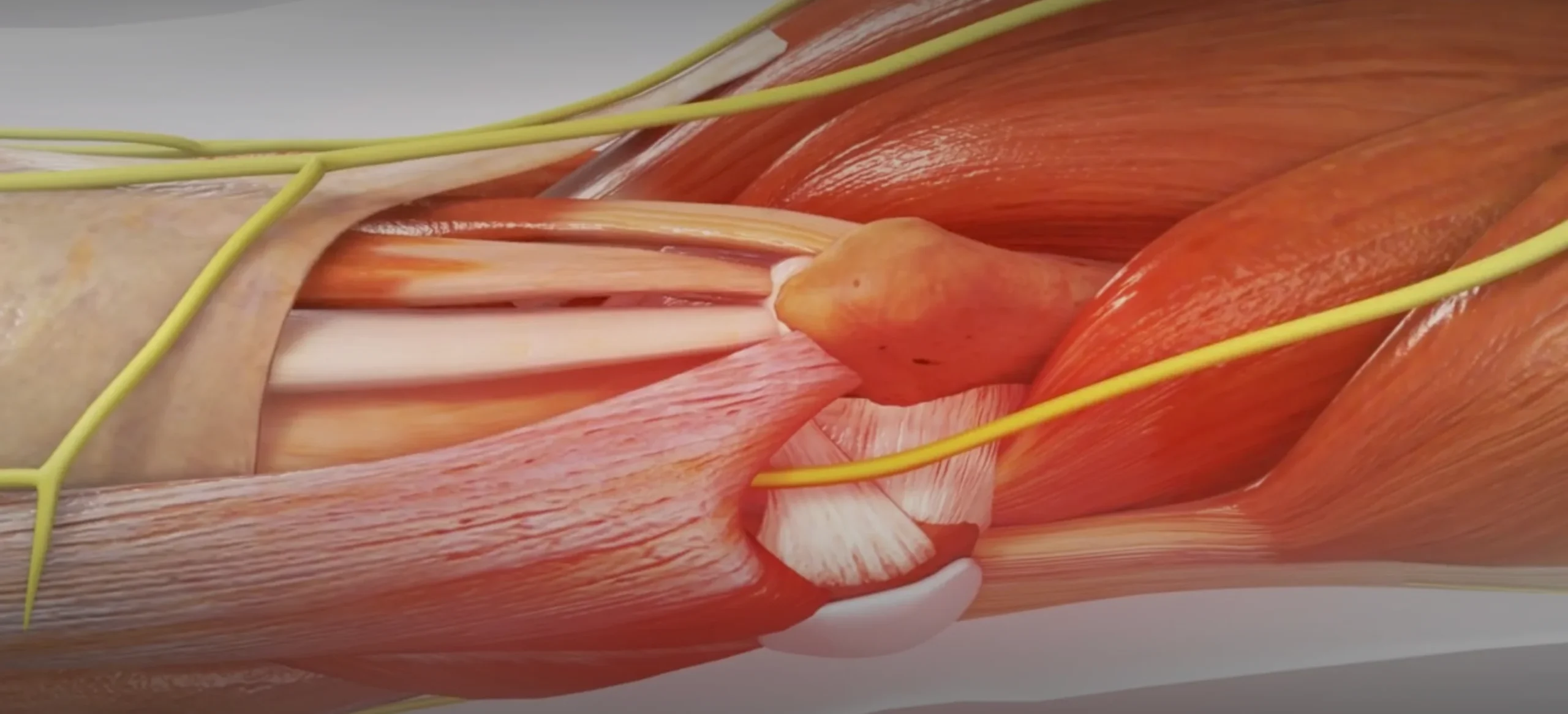
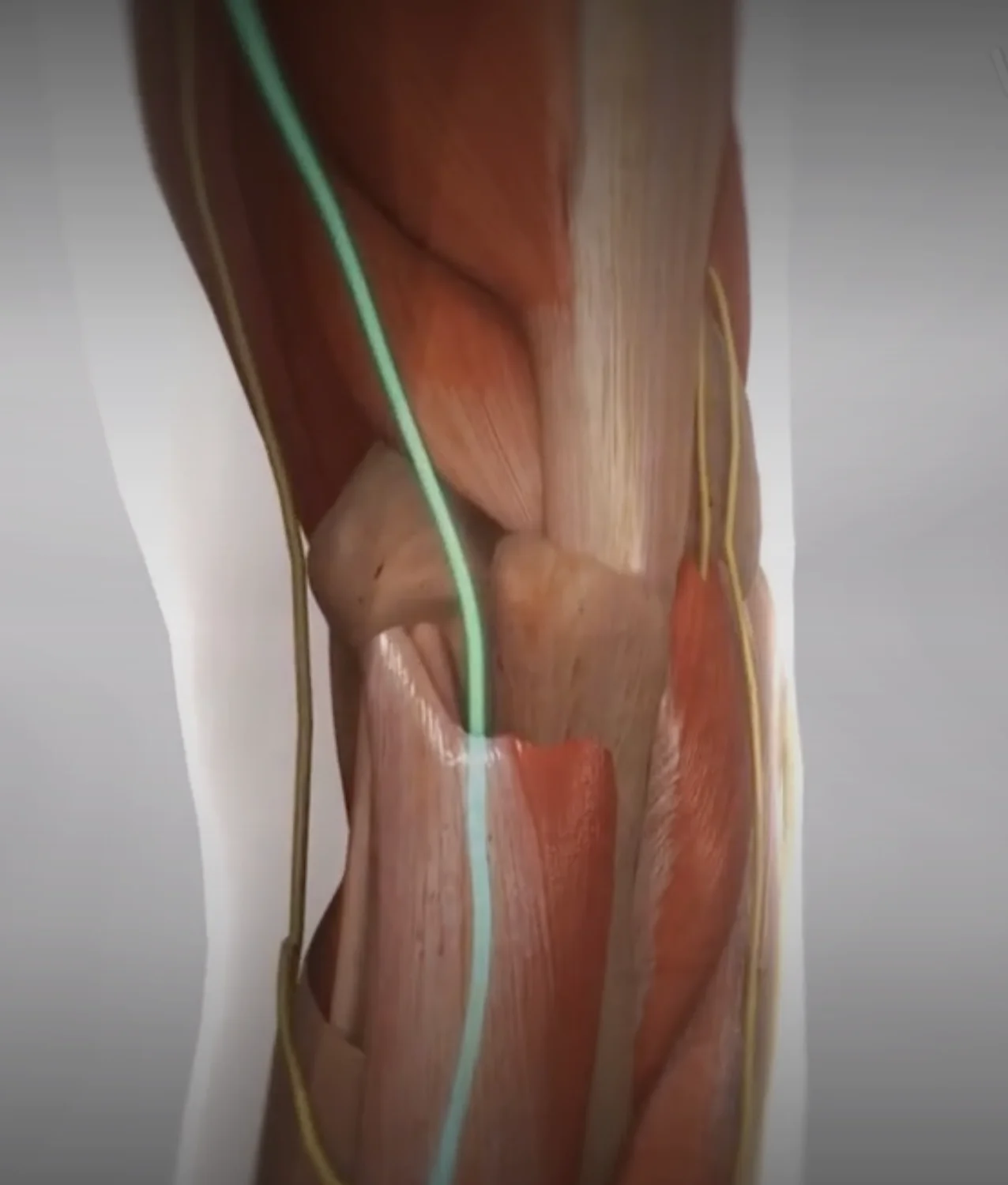
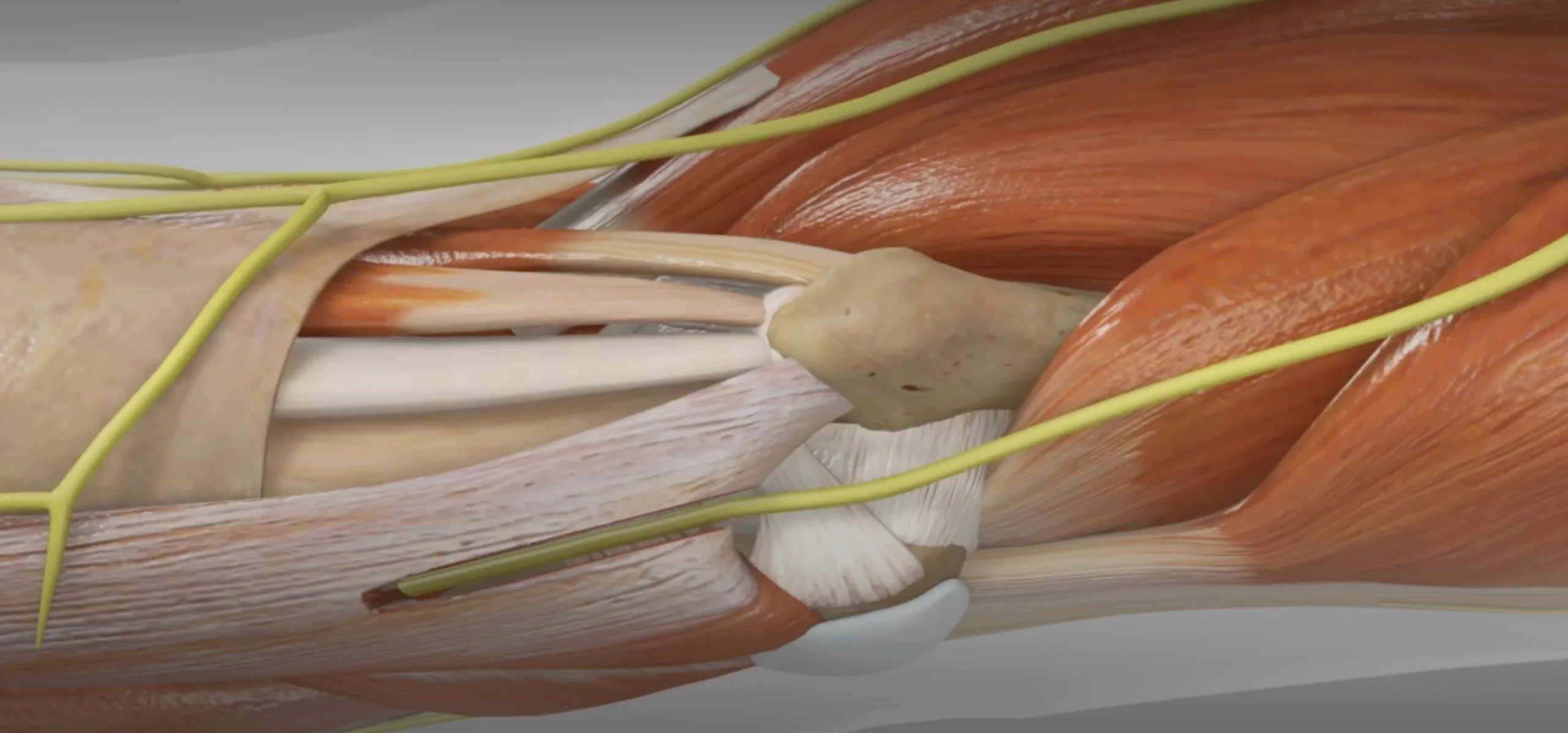
Cubital tunnel syndrome is a peripheral nerve entrapment condition affecting the ulnar nerve at the elbow. The ulnar nerve passes through the cubital tunnel, a narrow passageway formed by bone, muscle, and tissue on the inner side of the elbow. This condition occurs when the ulnar nerve becomes compressed or irritated at this location.
The condition commonly presents with numbness and tingling in the ring and small fingers, particularly during activities involving elbow flexion. Patients may experience weakness in grip strength and difficulty with fine motor tasks. Symptoms often worsen at night or with prolonged elbow flexion. Advanced cases may present with intrinsic muscle wasting in the hand and permanent sensory changes.
Risk factors include repetitive elbow flexion, direct pressure on the elbow, trauma, and occupational activities requiring prolonged elbow flexion or forceful gripping. Workers in industries requiring repetitive arm movements, such as assembly line workers or those using vibrating tools, are particularly susceptible.
Diagnosis primarily relies on clinical examination, including assessment of sensory changes in the ulnar nerve distribution and muscle strength testing. Provocative tests include the elbow flexion test and Tinel’s sign at the cubital tunnel. Electrodiagnostic studies, including nerve conduction studies and electromyography, can confirm the diagnosis and determine the severity of nerve compression.
Conservative management includes activity modification, ergonomic adjustments, and night splinting to maintain elbow extension. Patient education focuses on avoiding prolonged elbow flexion and direct pressure on the nerve. Physical therapy may help with nerve gliding exercises and strengthening of surrounding muscles.
Surgical intervention is considered when conservative measures fail or in cases with persistent symptoms, muscle weakness, or evidence of nerve damage. Surgical options include in-situ decompression, anterior transposition of the ulnar nerve (subcutaneous, intramuscular, or submuscular), and medial epicondylectomy. The choice of surgical technique depends on individual patient factors and surgeon preference.
Post-operative rehabilitation includes protected mobilization and gradual return to activities. Most patients experience improvement in symptoms, though recovery may be prolonged in cases with severe or chronic compression. Complete resolution of symptoms is more likely when intervention occurs before permanent nerve damage develops.
Prevention strategies include workplace ergonomic modifications, proper positioning during sleep and daily activities, and awareness of activities that may compress the nerve. Regular breaks from repetitive activities and maintaining good posture can help reduce the risk of developing or exacerbating symptoms.
Prognosis varies depending on the severity and duration of compression, timing of intervention, and patient compliance with treatment recommendations. Early recognition and appropriate management are crucial for optimal outcomes. Long-term monitoring may be necessary to prevent symptom recurrence and ensure sustained improvement.
Cubital tunnel syndrome is a common peripheral neuropathy affecting the ulnar nerve at the elbow. The condition arises from compression or irritation of the nerve as it passes through the cubital tunnel, a narrow passageway formed by bony and ligamentous structures.
Patients typically present with paresthesia and numbness in the ring and small fingers, along with weakness in grip strength and intrinsic hand muscles. Pain along the medial elbow, sometimes radiating distally, is common. Physical examination may reveal a positive Tinel’s sign at the cubital tunnel and Froment’s sign indicating thumb adduction weakness. In advanced cases, clawing of the ring and small fingers may be observed.
Diagnosis relies primarily on clinical presentation, supported by provocative tests such as the elbow flexion test. Electrodiagnostic studies can confirm the diagnosis and assess severity. Differential diagnoses include cervical radiculopathy and thoracic outlet syndrome.
Management follows a stepwise approach, beginning with conservative measures: Patient education on avoiding prolonged elbow flexion; Nighttime splinting; Activity modification; Ergonomic adjustments; NSAIDs for pain relief; Physical therapy
If conservative treatment fails, surgical options include: In situ decompression, Anterior transposition, and or medial epicondylectomy. Dr. McCormick prefers in-situe decompression.
Post-operative rehabilitation is crucial for optimal outcomes and is general quick. The prognosis is generally favorable with appropriate management, though recovery can be prolonged in severe cases. Prevention strategies focus on ergonomic awareness and early symptom recognition.
Cubital Tunnel Syndrome occurs when the ulnar nerve — the nerve that gives sensation to the ring and little fingers — becomes compressed as it passes through a tight space on the inside of the elbow called the cubital tunnel. When irritated or compressed, the nerve can cause:
The ulnar nerve is the same nerve that causes the “funny bone” sensation. When it’s compressed repeatedly or for long periods, symptoms can progress and eventually affect daily function, sleep, work tasks, or sports performance.
Cubital Tunnel Syndrome can be caused by structural, positional, or repetitive stress on the elbow. Common contributing factors include:
Over time, this constant bending-and-compression stretches the ulnar nerve like a rope rubbing over a corner — eventually irritating or damaging it.
SIGMA Orthopedics does not treat nerve compression like a routine condition — we follow a comprehensive, data-driven, symptom-specific pathway designed to optimize long-term nerve health.
Our approach includes:
A thorough assessment may include:
We match treatment to severity — choosing the least invasive, most effective option.
Patients are guided through a structured recovery plan focusing on:
We use validated patient-reported outcome measures to monitor improvement and prevent long-term deficits.
Our team coordinates therapy, bracing, follow-up, and recovery logistics — ensuring the entire process is seamless.
Many patients improve without surgery if treated early. Options include:
Keeping the elbow slightly extended at night to minimize nerve stretch during sleep.
Avoiding leaning on the elbow or prolonged bending.
Ice, oral medication, or localized treatments to reduce swelling.
Modifying biomechanics to reduce nerve strain.
If symptoms persist or worsen, especially if weakness is present, surgery may be recommended.
If the nerve is significantly compressed or symptoms are not improving, a cubital tunnel release may be the most effective treatment.
The procedure is typically outpatient and may include:
Releasing the tight structures in the cubital tunnel to allow the nerve more space.
If the nerve is unstable or shifts out of position, it may be gently moved to a more protected location in front of the elbow.
Removing a small portion of bone to prevent nerve irritation.
The choice depends on elbow anatomy, nerve stability, and surgeon evaluation.

Most patients experience:
Nerve healing continues over 6–12 months for many patients.
Whether you’re a desk worker, athlete, tradesperson, musician, or weekend warrior — we match treatment to your demands.
You should contact us promptly if you experience:
If managed early, outcomes are typically excellent.

If you’re experiencing numbness, tingling, pain, or weakness from possible Cubital Tunnel Syndrome, don’t delay evaluation. Early intervention can protect nerve health and prevent long-term functional loss.