At SIGMA Orthopedics & Sports Medicine, we recognize that chronic elbow tendon pain — from conditions like tennis elbow, golfer’s elbow, or chronic tendinopathy — can not only limit your performance, but also affect quality of life: from everyday tasks to work, hobbies, or sports. Rather than relying solely on pain pills, steroid shots, or surgery, our Regenerative Medicine program offers a more natural, biologic-driven pathway aimed at healing the tendon — not just masking pain.
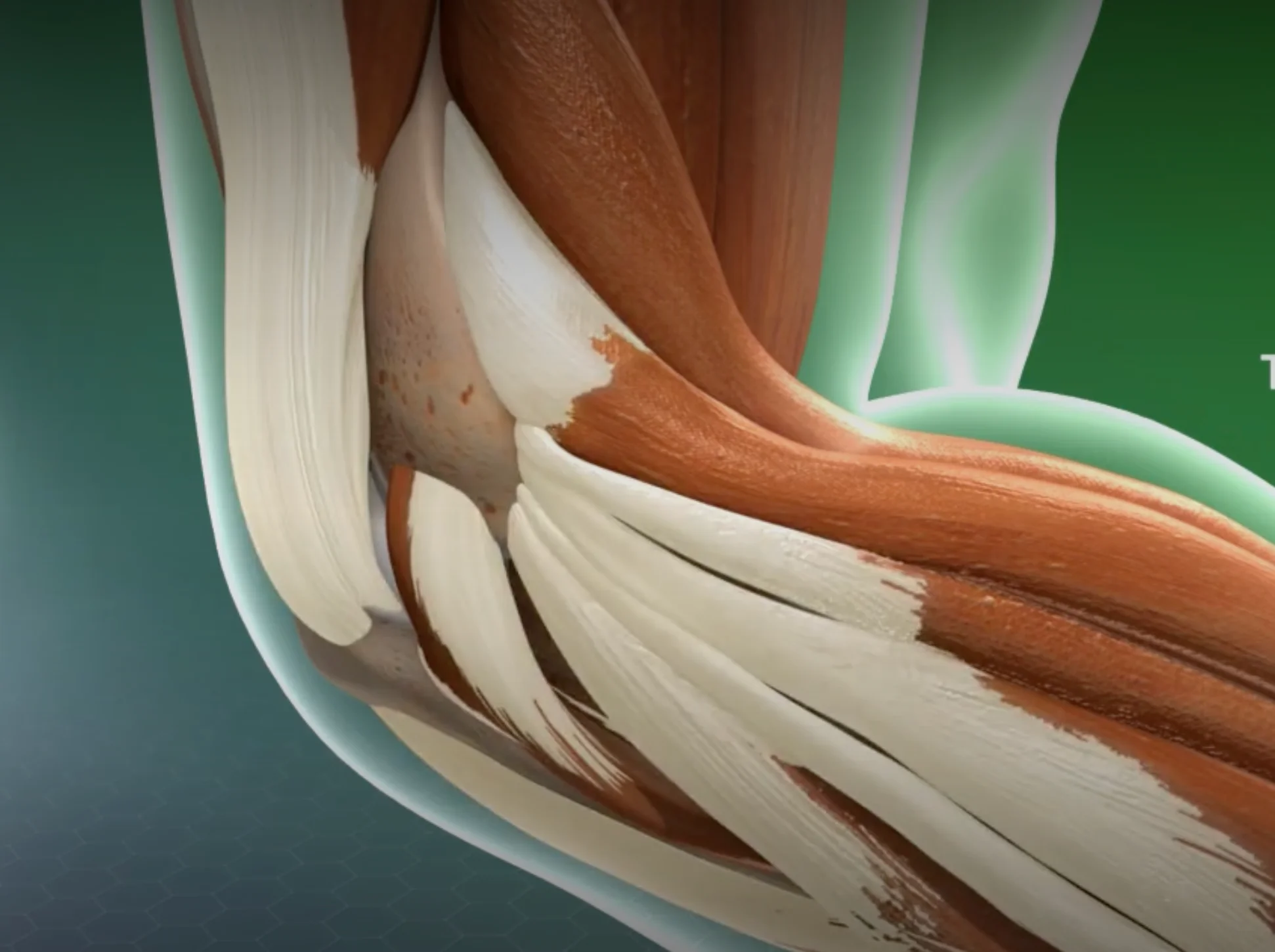
Tennis elbow — also known as lateral epicondylitis or tendinopathy — is one of the most common and frustrating causes of elbow pain. It’s not simply “inflammation.” In many patients, the tendon fibers at the outside of the elbow weaken over time, losing strength, flexibility, and the ability to heal on their own.
At SIGMA Orthopedics & Sports Medicine, we treat this condition using a precise, data-driven, and biologically intelligent approach. Rather than relying on repeated steroid injections or long periods of rest, we use advanced orthobiologic treatments like PRP or BMAC to stimulate real tendon repair at the cellular level — helping patients return to work, sport, and daily life with restored strength and durability.
This short video walks you step-by-step through:
If you’re struggling with persistent elbow pain, stiffness, or weakness — or if physical therapy and injections haven’t fully helped — this video will give you a clear look inside the SIGMA method and how we personalize regenerative care to help you get better, faster.
A small sample of the patient’s blood is drawn, then centrifuged to concentrate platelets and growth factors. This concentrate is injected into or around the injured tendon. Platelets release growth factors that can accelerate tissue healing and reduce inflammation.
Bone marrow (typically from the iliac crest/hip bone) is aspirated under sterile conditions, then processed to concentrate mesenchymal stem cells and growth factors. The resulting BMAC is then injected under imaging guidance (ultrasound or fluoroscopy) to the injured area.
Outline the rationale and potential benefits:
Local anesthesia (or light sedation), sterile preparation, ultrasound-guided injection of PRP or BMAC into/around the tendon. The whole procedure is typically done in-office and takes under an hour.
While individual results vary, many patients begin to notice gradual improvement in pain, function, and strength over several weeks to a few months. Full benefit may take 8–12 weeks.

Define the ideal patient profile to guide referrals / patient self-screening:

Leverage credentials, brand (SIGMA), and unique approach:
