Understanding, Diagnosing, and Treating Nerve Pain with Precision
At SIGMA Orthopedics, we take a fighter-pilot approach to spine care: identify the exact problem, eliminate uncertainty, and deliver predictable results. If neck pain, arm numbness, or radiating nerve symptoms are disrupting your life, our evidence-based diagnostics and tailored treatments can help you recover—confidently and efficiently. Schedule an appointment or request an MRI review today.
Cervical radiculopathy—often called a “pinched nerve in the neck”—happens when a nerve root in the cervical spine becomes compressed or irritated. This can cause pain, numbness, tingling, or weakness that travels from the neck into the shoulder, arm, or hand.
At SIGMA Orthopedics & Sports Medicine, we treat cervical radiculopathy with a precision-based, minimally invasive, data-driven approach. Our goal is to identify the exact source of nerve irritation and build a personalized pathway to relief and full functional recovery.
Your cervical spine is made of seven vertebrae (C1–C7). Between each vertebra is an intervertebral disc—a shock-absorbing cushion that helps you bend and rotate. Over time, discs can bulge, herniate, or degenerate, pressing on nearby nerve roots.
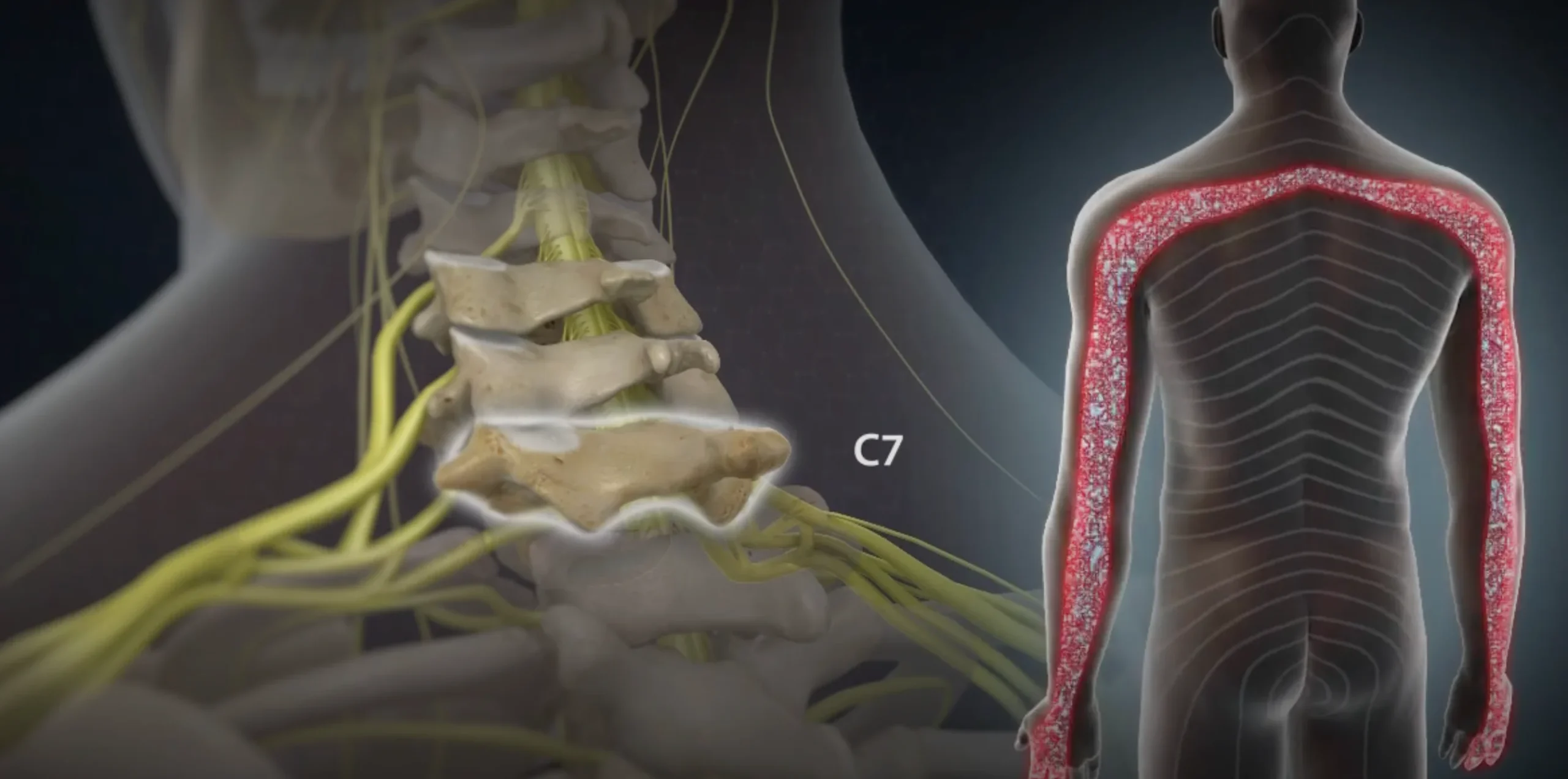
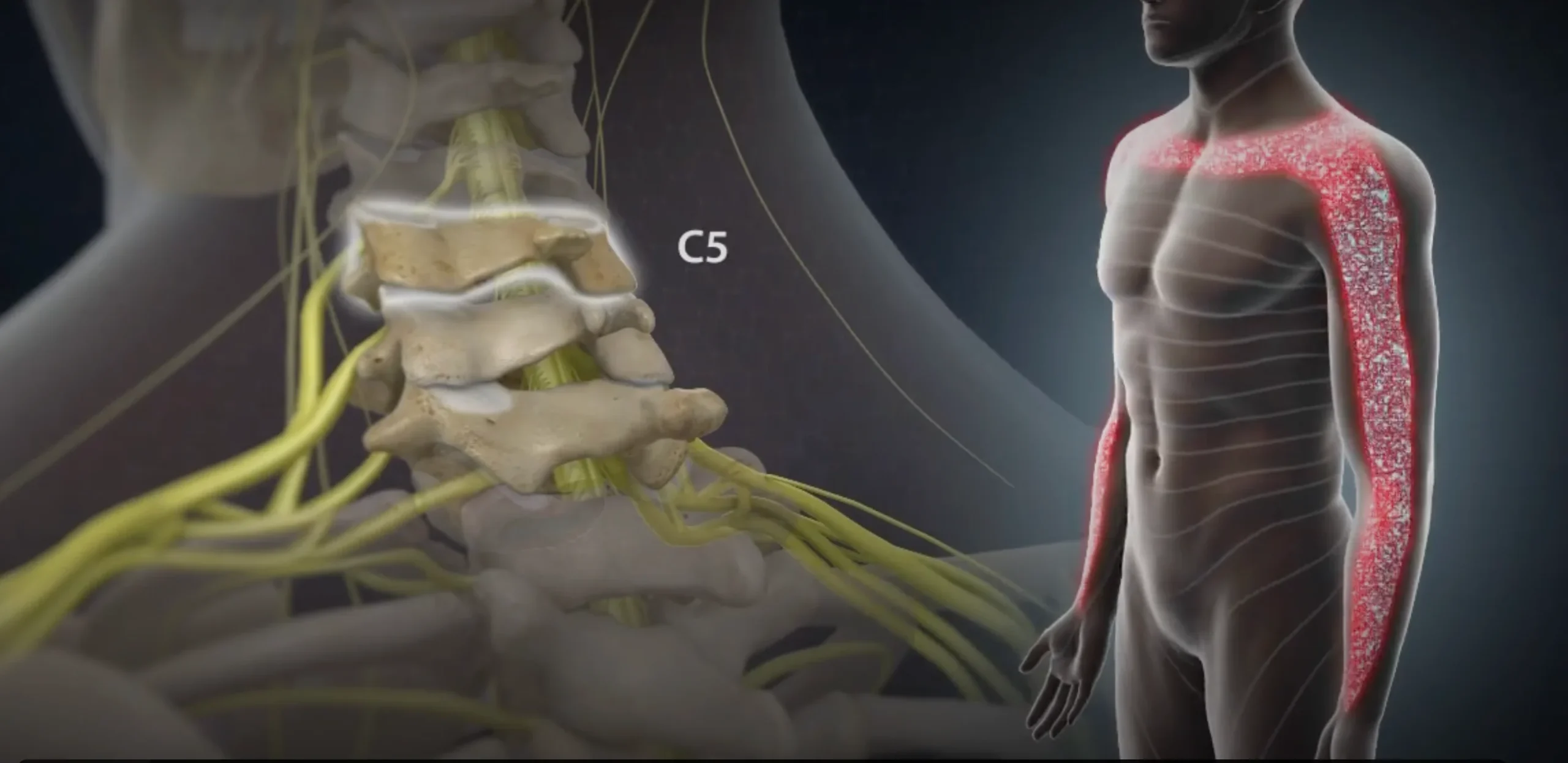
Nerves leave your spinal cord through small openings called foramina. When these openings narrow from disc collapse, arthritis, or bone spurs, the nerves can become pinched—causing radiculopathy.
Facet joints and ligaments stabilize the spine. With age, they can thicken or develop arthritis, contributing to foraminal stenosis or nerve compression.
When any of these structures encroach on a nerve root, symptoms follow the path of that nerve—into the shoulder, upper arm, forearm, or hand.
A herniated disc can protrude and compress a nerve root, often causing sharp, radiating arm pain.
Age-related wear leads to disc height loss, bone spurs, and joint overgrowth—narrowing the space available for nerves.
When the nerve’s exit channel narrows, even normal motion can irritate or compress the nerve.
Whiplash injuries, repetitive overhead activity, or heavy lifting can accelerate degenerative changes.
Chronic forward-head posture, prolonged screen use, or muscular imbalance can overload spinal structures.
When the nerve’s exit channel narrows, even normal motion can irritate or compress the nerve.
Symptoms depend on the specific nerve root involved but commonly include:
If you’re unsure whether your symptoms represent a “pinched nerve,” our team can assess and confirm this during a single visit.
Common nerve patterns:
If symptoms progress or weakness develops, early evaluation is important.

We assess which movements reproduce symptoms, evaluate motor strength, test reflexes, and map sensory changes.
Imaging helps identify disc herniation, foraminal narrowing, bone spurs, or structural instability
Not everything seen on MRI causes symptoms. We only treat what matches your actual pattern.
Selective nerve-root injections or foraminal blocks can confirm the exact level causing pain.
This structured diagnostic process ensures accuracy, safety, and appropriate treatment—avoiding unnecessary injections or surgery.
Every patient receives a customized recovery plan supported by digital education, remote tools, and clear checkpoints for progress.

Seek urgent evaluation if you experience:

Cervical radiculopathy is highly treatable when diagnosed accurately and managed with precision. Whether you’re struggling after trauma, dealing with chronic neck pain, or trying to understand what your MRI means, SIGMA is here to guide you with clarity and confidence.
- Significant nerve compression
- Progressive weakness
- Persistent pain despite conservative care
Options include:- Microsurgical decompression
- Cervical disc replacement (motion-preserving)
- ACDF fusion when stability is required
Our surgical philosophy prioritizes minimal tissue disruption, precision correction, and rapid return to daily life.